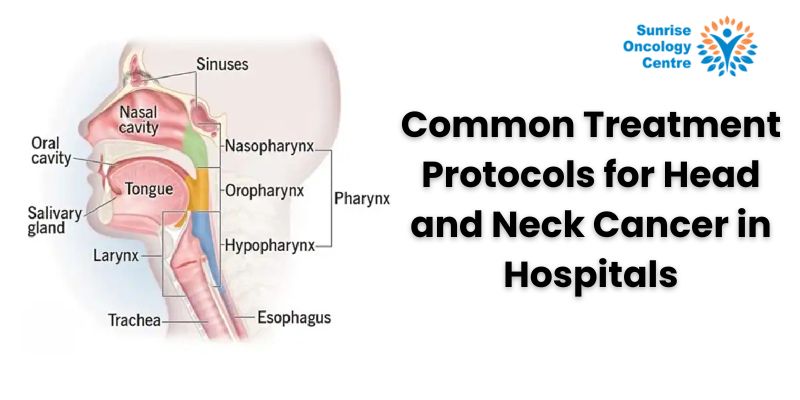
Head and neck cancer treatment protocols have evolved significantly over the past few decades, providing hope and effective solutions for patients diagnosed with this challenging disease. Head and neck cancers include cancers of the mouth, throat, larynx, nasal cavity, and salivary glands. They require a multidisciplinary approach for optimal outcomes. In this article, we will explore various treatment protocols available, focusing on their effectiveness, advancements, and what patients can expect during their treatment journey.
Understanding head and neck cancer treatment
Head and neck cancers arise from the squamous cells that line the moist mucosal surfaces inside the head and neck. These cancers are often linked to risk factors such as tobacco use, alcohol consumption, and human papillomavirus (HPV) infection. Early detection is crucial for improving survival rates, making awareness and regular screenings vital.
Diagnostic Procedures: Diagnosis typically starts with a physical examination and a review of the patient’s medical history. Imaging studies such as CT scans, MRIs, and PET scans are used to determine the extent of the cancer. Biopsies are performed to confirm the diagnosis and to identify the specific type of head and neck cancer.
Surgical Interventions: Surgery is often the first line of treatment for many types of head and neck cancers. Different surgical procedures may be recommended depending on the location and stage of the cancer. These include:
Tumor Resection: Removal of the tumor and some surrounding healthy tissue to eliminate all cancerous cells.
Neck Dissection: Removal of lymph nodes in the neck to prevent the spread of cancer.
Reconstructive Surgery: Post-tumor removal and reconstructive surgery may be necessary sometimes to restore appearance and functionality.
Surgical interventions have advanced techniques such as minimally invasive surgery and robot-assisted surgery, which offer reduced recovery times and improved precision.
Radiation Therapy: Radiation therapy uses high-energy radiation to destroy cancer cells. It is often used in conjunction with surgery or as a standalone treatment when surgery is not viable. There are different types of radiation therapy:
External Beam Radiation: This is the most common form, where beams are directed at the tumor from outside the body.
Brachytherapy: Involves placing radioactive material directly inside or near the tumor.
Radiation therapy can effectively shrink tumors and kill cancer cells, but it also comes with side effects such as skin irritation, fatigue, and difficulty swallowing.
Chemotherapy: Chemotherapy involves the use of drugs to kill cancer cells. It can be administered orally or intravenously and is often used in combination with radiation therapy (chemoradiation) to enhance effectiveness. Chemotherapy is typically recommended for advanced stages of head and neck cancer or when the cancer has spread to other parts of the body.
Targeted Therapy: Targeted therapy is a newer approach that focuses on specific molecules involved in cancer growth. By targeting these molecules, the therapy can effectively inhibit cancer cell proliferation while minimizing damage to normal cells. This therapy is often used when other treatments are not effective or in conjunction with chemotherapy and radiation therapy.
Immunotherapy: Immunotherapy leverages the body’s immune system to fight cancer. This treatment has shown promise in treating various types of cancers, including head and neck cancers. Immune checkpoint inhibitors help the immune system recognize and attack cancer cells. Immunotherapy can be especially beneficial for patients with recurrent or metastatic head and neck cancers.
Clinical Trials and Emerging Treatments: Researchers continuously explore new therapies and combinations to improve the effectiveness of head and neck cancer treatment protocols. Patients should discuss with their oncologists the possibility of joining clinical trials to access these innovative treatments if they are available and accessible in their vicinity.
Managing Side Effects and Quality of Life
Head and neck cancer treatment can significantly impact quality of life. Managing side effects is a critical aspect of the treatment protocol. Supportive care measures include:
- Nutritional Support: Ensuring patients maintain adequate nutrition despite difficulties in eating and swallowing.
- Pain Management: Addressing pain through medications and alternative therapies.
- Speech and Swallowing Therapy: Helping patients regain functionality post-treatment.
- Psychosocial Support: Providing mental health support to cope with the emotional challenges of cancer treatment.
Follow-up Care: Regular follow-up care is essential to monitor for recurrence signs and manage long-term side effects. Follow-up visits typically include physical exams, imaging tests, and sometimes blood tests to ensure the cancer has not returned.
Head and neck cancer treatment protocols have advanced, offering patients multiple avenues for effective treatment and improved survival rates. From surgery and radiation to chemotherapy, targeted therapy, and immunotherapy, each treatment plan is tailored to the patient’s individual needs. Understanding these options and working closely with your healthcare team can help patients confidently navigate their treatment journey.